Hi Friend!
We live in a world that revolves around all things social media. It takes little to no effort to look something up and we can connect to our friends, family, and celebrities alike with the simple swipe of a screen.
While this interconnectedness presents many advantages, having a wealth of information so easily accessible has created new concerns about what kind of information is being shared.
Accurate information is a cornerstone in healthcare, and it’s particularly crucial in women’s health. The online world is a mix of advice, quick fixes, personal stories, and trending “health hacks” that often outpace verified medical facts.
While some content is harmless, a growing amount of misinformation can be a dangerous detour, delaying proper diagnosis, worsening symptoms, or leading women towards unsafe treatments. This is why critical evaluation of online content is not only necessary but also empowering and responsible.
From social media myths about fertility and hormones to misleading claims about birth control, menopause, or gynecologic conditions, this wave of misinformation has significant, real-world consequences that you need to be aware of and cautious about.
At a recent Menopause Society conference, I was taken aback by the sheer pervasiveness of social media misinformation about menopause hormone therapy (commonly referred to as hormone replacement therapy or HRT). The extent of this issue is truly alarming and underscores the urgent need for critical evaluation of online health information.
THE NUMBERS.
It’s essential to preface this discussion with the disclaimer that I am not arguing that someone should disregard medical information found on social media channels.
In fact, I would say that social media has been an excellent tool in sparking conversations between patients and physicians that might not have otherwise occurred.
I can’t stress enough how critical it is to be alert and engaged, using discernment when taking in the endless flow of information about menopause hormone treatment.
A recent study published in September 2025 by BMJ Open presented some eye-opening numbers:
- In 2021/2022, 7.8 million items for hormone replacement therapy (HRT) were prescribed, a rise of 35% compared with the 12 months before.
- Google Trends shows an increase in popularity in searches for ‘HRT’ in the UK over the last 5 years.
- A search on Instagram in April 2022 revealed half a million posts referencing #HRT, with the top 10 posts on TikTok referencing HRT collectively viewed over 2 million times.
- 84.4% of the adult UK population uses social media. 85% of UK women use content creation sites like YouTube (63%), Instagram (56%), Twitter (37%), and TikTok (12%).
- The number of articles about menopause in newspapers has quadrupled in the last decade, and over a third of postmenopausal women seek information on menopause from social media, including YouTube.1
So why are these numbers so eye-opening?
Because it pulls back the curtain on just how much information (accurate or not) is readily available across social media channels and how many women are potentially consuming it.
These two factors alone significantly raise the stakes in terms of vetting sources.
the study.
The NICE (National Institute for Health and Care Excellence) and the MHRA (Medicines and Healthcare Products Regulatory Agency) via the BNF (British National Formulary) were searched for guidance applicable during the study period (1 January 2022 to 1 May 2024) for:
(1) indications for HRT (Hormone replacement therapy), including for the prevention of future ill health;
(2) adverse effects of HRT;
(3) indications for testosterone for menopause.
This information served as the standard for comparing social media posts.
The NICE and BNF indications for HRT included: vasomotor symptoms, mood disorders, and urogenital symptoms, with testosterone recommended ‘for altered sexual function, seeking specialist advice on the appropriateness of testosterone supplementation (off-label indication)’.
The BNF also noted that ‘estrogen, given systemically in the perimenopausal and postmenopausal period…also diminishes postmenopausal osteoporosis, but other drugs are preferred’.
They also stated ‘The MHRA advises that HRT should only be prescribed to relieve postmenopausal symptoms that are adversely affecting quality of life and treatment should be reviewed regularly to ensure the minimum effective dose is used for the shortest duration.’ 2
These standards serve as the metric for comparing social media posts during the subsequent examination.
the data.
Data were extracted from 180 sources, with 30 from each of the six platforms (Facebook, Google, Instagram, TikTok, Twitter (X), YouTube).
HRT recommendations that were incongruent with NICE and BNF recommendations included:
- prevention of cardiovascular disease or memory impairment
- cognitive benefits
- improvement of hair and skin appearance
- improvement in palpitations
- anxiety
- weight control (including weight loss)
- musculoskeletal benefits
- energy
- overall well-being
Testosterone recommendations that were incongruent with NICE and BNF recommendations included:
- improvement in energy
- motivation
- cognitive function
- sleep
- musculoskeletal benefits
- weight control
- well-being
- hair and skin appearance
- anxiety
- mood
The majority (67.2%) of all recommendations analyzed were incongruent with NICE/BNF recommendations.
That means that over two-thirds of the data in this study contradicted the current medical recommendations.
Two. Thirds.
Not only is that concerning, but it is consequential.
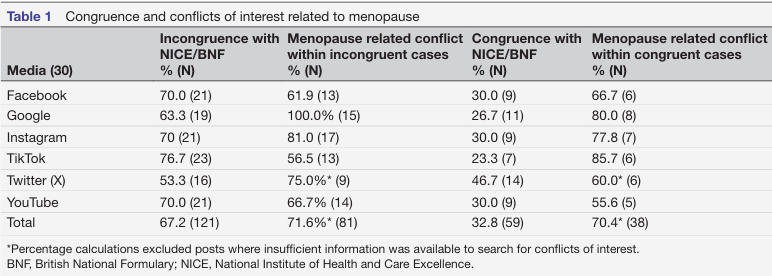
Infographic Source
McCartney M, Morgan-Young R, Sullivan F, et al. Does online information about hormone replacement therapy (or menopause hormone therapy) reflect indications from the British National Formulary and guidance from the National Institute for Health and Care Excellence: a cross-sectional study of UK media. BMJ Open 2025;15: e094773.
Infographic Source
McCartney M, Morgan-Young R, Sullivan F, et al. Does online information about hormone replacement therapy (or menopause hormone therapy) reflect indications from the British National Formulary and guidance from the National Institute for Health and Care Excellence: a cross-sectional study of UK media. BMJ Open 2025;15: e094773.
the source.
Have you ever heard someone say one of these phrases: “Consider the source”, “Take it with a grain of salt”, or “Don’t take it at face value”?
All these sayings encourage critical thinking, regardless of their context, and medical advice or information from social media is no exception.
Not only is it essential to consider the source of information, but it’s also important to consider the motivation behind what is shared.
The quality of your medical decisions depends heavily on the quality of the information you use. Online content varies widely—some is written by trained clinicians using evidence-based guidelines. At the same time, other material comes from influencers, advertisers, or anonymous users with little to no medical background.
Considering the source is crucial because reliable medical guidance should be grounded in research, clinical experience, and established standards of care. Trusted sources—such as licensed providers, professional medical organizations, and peer-reviewed publications—offer information that is vetted for accuracy and safety.
In contrast, unverified sources may promote myths, oversimplify conditions, or push products rather than facts.
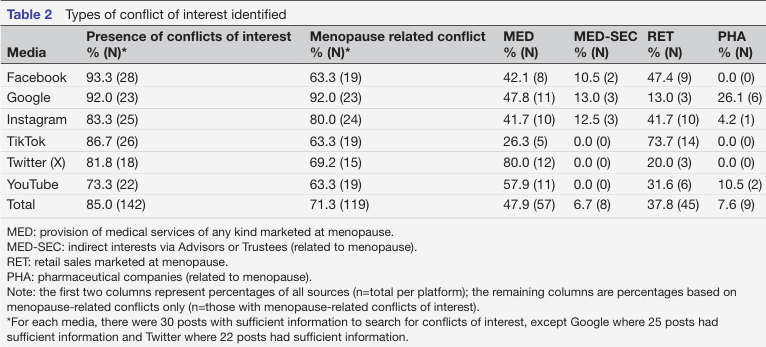
The BMJ Open study identified conflicts of interest among publicly available social media posts related to menopause hormone therapy.
A conflict of interest occurs when a person or organization sharing medical information has a financial, professional, or personal stake in the audience’s decisions. When this happens, the accuracy and objectivity of the information can become compromised. The study then further qualified the conflict of interest into four categories:
- Direct conflict via paid-for medical products (e.g., private healthcare clinics, including those specifically advertising menopause consultations).
- Direct conflict via retail products (advertised services to specifically menopausal women, for example, dietary packages, cosmetics, health and food supplements, exercise classes, coaching).
- Direct funding from a pharmaceutical company (e.g., payments by a manufacturer of interventions for menopause).
- Funded indirectly, through advisors, trustees, or managers (via advisory or consultancy roles to industry or directly supported by the pharmaceutical industry (e.g., via sponsorship or fees to individuals)3
Conflicts of interest can lead to biased explanations, selective presentation of data, or recommendations that prioritize profit or personal agenda over patient well-being. Overstating benefits, downplaying risks, or steering people toward specific treatments, supplements, or procedures that may not be necessary or appropriate can all be effects of these conflicts of interest.
The result is reduced trust, distorted decision-making, and potential harm if individuals act on advice that lacks evidence-based support. Recognizing conflicts of interest helps patients evaluate information more critically.
It ensures their health decisions are guided by evidence—not by someone else’s incentives.
The lack of truly independent advice online was noted, that is, that which had no commercial alignment or affiliation.
This is important because such information does exist, but it was not prominent on the websites searched in the study. 4
the fallout.
Believing inaccurate medical information on social media can lead to a cascade of consequences that affect both personal health and the broader public health.
When misleading posts, oversimplified claims, or unproven “quick fixes” are treated as truth, people may delay proper medical care, misinterpret symptoms, or choose ineffective treatment or, worse, even harmful ones, which can exacerbate existing conditions, instill unnecessary fear, or provide false reassurance when urgent attention is required.
Beyond individual risks, widespread acceptance of misinformation erodes trust in qualified healthcare professionals, fuels stigma around sensitive women’s health issues, and can contribute to harmful trends like improper supplement use, DIY medical procedures, or avoidance of evidence-based screenings.
Over time, this collective confusion makes it increasingly difficult for accurate information to stand out, allowing misinformation to spread more rapidly and reach more vulnerable groups.
the proactive approach.
You may be thinking, ok, Farris, this is all great information, but how do I know how to vet what I’m reading as reliable?
I’m so glad you asked.
Avoiding medical misinformation on social media begins with slowing down and approaching every post—whether shared by friends, influencers, or seemingly trustworthy pages—with healthy skepticism.
Before accepting a claim as accurate, check the source. Is it a licensed healthcare professional, a reputable medical organization, or a peer-reviewed publication?
Look for evidence, not anecdotes: credible posts will cite studies, acknowledge limits, and avoid dramatic, one-size-fits-all promises. It also helps to compare information across multiple reliable outlets; if only one account is making a bold claim, that should be a red flag.
Pay attention to emotional language, sensational headlines, and posts that promote products or treatments, as these often signal bias or a financial motive.
Finally, when in doubt, consult a qualified healthcare provider who can confirm whether the information aligns with real medical guidance.
By being intentional, curious, and cautious about what you read online, you can help protect yourself from misinformation that may lead to confusion, delayed care, or harmful health decisions.
My content may not always be the flashiest, trendiest, or most entertaining on your feed, but it is intentional. I care about accuracy over hype. Women’s health deserves clarity, not catchy misinformation.
I’m committed to providing information that is responsible, evidence-based, and genuinely helpful.
So, if that means choosing truth over trends or education over entertainment, it’s a trade I’m willing to make. Your health and your trust matter more than going viral.
If you have questions or concerns about your hormones, please call the clinic at 405-701-6717 to make an appointment. We would be honored to walk with you through this journey!
With Love,
Dr. Ronni Farris
- McCartney M, Morgan-Young R, Sullivan F, et al. Does online information about hormone replacement therapy (or menopause hormone therapy) reflect indications from the British National Formulary and guidance from the National Institute for Health and Care Excellence: a cross-sectional study of UK media. BMJ Open 2025;15:e094773. ↩︎
- BMJ Open 2025;15: e094773. ↩︎
- McCartney M, et al. BMJ Open 2025;15: e094773 ↩︎
- McCartney M, et al. BMJ Open 2025;15: e094773 ↩︎
*Medical Disclaimer
The information provided by Ronni E. Farris, MD Gynecology, Wellness & Aesthetics (“we,” “us,” or “our”) on this website www.ronnifarrismd.com/blog (the “Website”) is for general informational purposes only. All content, including text, graphics, images, and information, is presented as an educational resource and is not intended as a substitute for professional medical advice, diagnosis, or treatment.
Please consult with a qualified healthcare provider before making any decisions or taking any action based on the information you find on this Website. Do not disregard, avoid, or delay obtaining medical or health-related advice from your healthcare provider because of something you have read on this Website.
This Website does not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on this website. Reliance on any information provided on the Website, its content creators, or others appearing on the website is solely at your own risk.
If you think you may have a medical emergency, call your doctor, go to the nearest emergency department, or call emergency services immediately. We are not responsible for any adverse effects resulting from your use of or reliance on any information or content on this Website.
By using this Website, you acknowledge and agree to this disclaimer in full.


Leave a Reply